Learn About Lung Auscultation
Educational resources for understanding breath sounds, their clinical significance, and proper auscultation techniques.
Introduction to Lung Auscultation
Auscultation is the act of listening to sounds within the body, typically using a stethoscope. In respiratory assessment, auscultation provides critical information about airflow through the tracheobronchial tree and the condition of surrounding lung tissue.
Historical Background
Lung auscultation was pioneered by René Laennec in 1816 when he invented the first stethoscope. Prior to this innovation, physicians would place their ear directly on the patient's chest to hear internal sounds, a practice known as immediate auscultation.
Modern Applications
Today, auscultation remains a fundamental skill in clinical practice, despite advances in imaging technology. It provides immediate information at the bedside, guides further testing, and helps monitor treatment response.
The Importance of Breath Sounds
Breath sounds are important clinical indicators that can reveal:
- Airflow patterns through the respiratory tract
- Presence of obstructions or narrowing in airways
- Accumulation of fluid or secretions in lung tissue
- Changes in lung density due to consolidation or collapse
- Inflammation of pleural membranes
Respiratory System Anatomy
Key Anatomical Structures
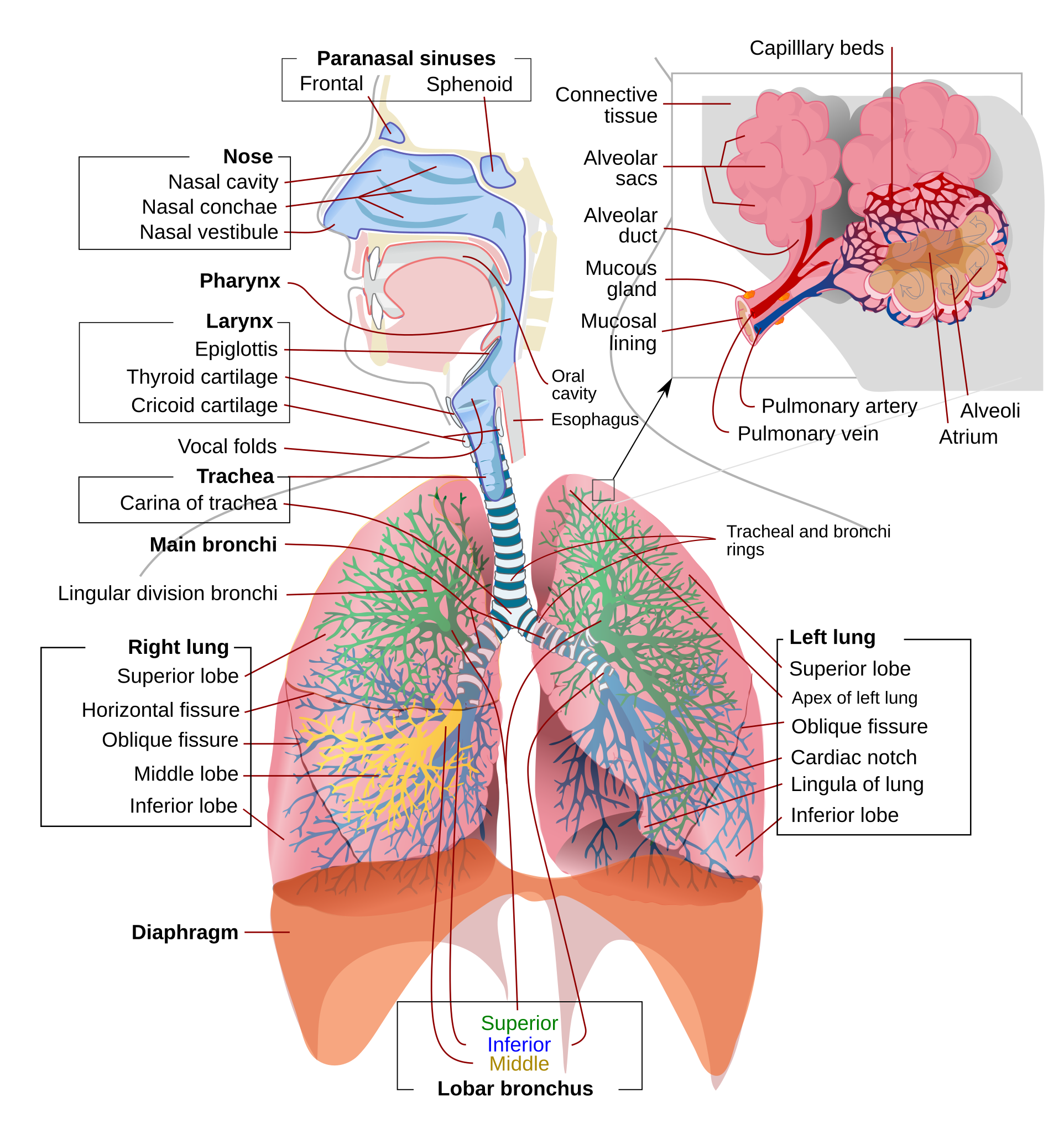
Upper Airway
The upper airway consists of the nose, pharynx, and larynx. These structures warm, filter, and humidify inspired air before it enters the lower airway.
Trachea
A cartilaginous tube extending from the larynx to the main bronchi, approximately 10-12 cm long in adults.
Bronchi and Bronchioles
The trachea divides into right and left main bronchi, which further branch into lobar bronchi, segmental bronchi, and eventually bronchioles. This branching creates a tree-like structure known as the bronchial tree.
Alveoli
Tiny air sacs (approximately 300 million per lung) where gas exchange occurs. The alveolar-capillary membrane allows oxygen to enter the bloodstream and carbon dioxide to be eliminated.
Lung Lobes
The right lung has three lobes (upper, middle, lower), while the left lung has two lobes (upper and lower). The left lung also contains the cardiac notch to accommodate the heart.
Pleura
A thin membrane that covers the lungs (visceral pleura) and lines the thoracic cavity (parietal pleura). The pleural cavity between these layers contains a small amount of lubricating fluid.
Normal Breath Sounds
Normal breath sounds are categorized into three main types based on their acoustic characteristics and the location where they are best heard:
Vesicular Breath Sounds
Soft, low-pitched, gentle "swooshing" sounds
Inspiration is 3 times longer than expiration (3:1)
Over most of the peripheral lung fields
Air moving through smaller airways and into alveoli
Bronchial Breath Sounds
Loud, high-pitched, hollow tubular sounds
Expiration is longer than inspiration (1:2)
Over the trachea and main bronchi (2nd-4th intercostal spaces)
Air moving through the large central airways
Broncho-vesicular Sounds
Medium-pitched sounds with intermediate qualities
Equal inspiratory and expiratory phases (1:1)
Upper anterior chest and posterior interscapular areas
Air moving through medium-sized airways
Auscultation Locations for Normal Breath Sounds
The type of breath sound you hear depends on where you place your stethoscope:
- Trachea and main bronchi: Bronchial sounds
- Upper anterior chest and between scapulae: Broncho-vesicular sounds
- Remainder of chest: Vesicular sounds
Important Notes
- Normal breath sounds can vary somewhat between individuals
- Intensity decreases with thick chest walls, obesity, or shallow breathing
- Elderly patients typically have diminished vesicular sounds due to decreased lung elasticity
- Finding bronchial sounds in peripheral lung fields indicates pathology
Abnormal Breath Sounds
Abnormal breath sounds, also called adventitious sounds, are additional sounds superimposed on normal breath sounds. They indicate various respiratory pathologies:
Wheezes
Description: Continuous, high-pitched, musical sounds resembling a whistle
Timing: Primarily heard during expiration, but can occur during inspiration in severe cases
Cause: Narrowed airways due to bronchoconstriction, mucosal edema, or external compression
Associated Conditions: Asthma, COPD, bronchitis, allergic reactions
Crackles (Rales)
Description: Discontinuous, non-musical, brief popping sounds
Timing: Usually heard during inspiration
Types: Fine crackles (high-pitched, brief) and coarse crackles (lower-pitched, longer)
Cause: Sudden opening of previously closed small airways or air bubbling through fluid
Associated Conditions: Pneumonia, pulmonary edema, pulmonary fibrosis, bronchiectasis
Rhonchi
Description: Continuous, low-pitched, rumbling or snoring-like sounds
Timing: Typically more prominent during expiration
Cause: Secretions or obstruction in larger airways
Associated Conditions: Chronic bronchitis, bronchiectasis, pneumonia with secretions
Note: Often clear or change after coughing
Stridor
Description: Loud, harsh, high-pitched monophonic sound
Timing: Primarily heard during inspiration
Cause: Partial obstruction of the upper airway (larynx or trachea)
Associated Conditions: Croup, epiglottitis, foreign body aspiration, vocal cord paralysis, laryngeal edema
Note: Often audible without a stethoscope; represents a medical emergency if acute
Pleural Rub
Description: Coarse, grating, creaking sound like leather rubbing together
Timing: Heard during both inspiration and expiration
Cause: Inflammation of pleural surfaces causing reduced lubrication between visceral and parietal pleura
Associated Conditions: Pleurisy, pleural inflammation due to pneumonia, pulmonary infarction, or rheumatologic conditions
Note: Not affected by coughing; may be painful for the patient
Absent or Diminished Breath Sounds
The absence or significant reduction of breath sounds in an area where they should be heard is also abnormal and may indicate:
- Pleural effusion
- Pneumothorax
- Severe emphysema
- Complete airway obstruction
- Atelectasis (lung collapse)
- Diaphragmatic paralysis
Proper Auscultation Technique
Preparation and Equipment
Stethoscope Selection
- Diaphragm: Use for high-pitched sounds (normal breath sounds, wheezes, fine crackles)
- Bell: Use for low-pitched sounds (some rhonchi, cardiac sounds)
- Ensure proper fit of earpieces (angled toward nose)
- Check that tubing is not too long (ideally less than 30cm)
Patient Preparation
- Ensure adequate exposure of chest (respect privacy)
- Position patient appropriately (usually sitting upright)
- Room should be quiet
- Warm the stethoscope diaphragm if cold
- Explain procedure to the patient
Auscultation Process
Breathing Instructions
- Ask patient to breathe slightly deeper than normal
- Instruct to breathe through the mouth
- Do not force hyperventilation which can cause light-headedness or altered breath sounds
- Listen through at least one complete respiratory cycle at each position
Systematic Approach
- Compare symmetrical points on both sides of the chest
- Start at the apices (tops) and work downward
- Follow a consistent pattern to avoid missing areas
- For posterior chest: examine from apex to base, side to side
- For anterior chest: examine from apex to base, side to side
Auscultation Landmarks
Anterior Chest
- Supraclavicular area: above clavicles
- Infraclavicular area: below clavicles
- Right middle lobe: right 4th-5th intercostal space
- Left lingular area: left 4th-5th intercostal space
- Lower lobes: 6th-7th intercostal spaces
Posterior Chest
- Upper lobes: above the scapular spines
- Interscapular area: between scapulae
- Lower lobes: below scapulae to 10th rib
- Bases: lowest accessible intercostal spaces
Lateral Chest
- Axillary region: upper portion
- Mid-axillary line: 4th-6th intercostal spaces
- Lower axillary region: down to 8th intercostal space
Common Pitfalls to Avoid
- Pressing too hard with the stethoscope, which can create artifacts
- Not comparing symmetrical points on both sides of the chest
- Auscultating through clothing, which muffles sounds
- Not allowing enough time at each location
- Confusing transmitted sounds (e.g., voice, heart) for lung sounds
- Not properly identifying anatomical landmarks
- Failing to ask the patient to breathe appropriately
- Rushing through the examination
Clinical Significance
Breath sounds are important clinical findings that help in the diagnosis and management of various respiratory conditions. Here are some key clinical correlations:
Common Conditions and Their Auscultation Findings
Asthma
- Expiratory wheezes throughout the lung fields
- Prolonged expiratory phase
- Wheezes that may clear with coughing or bronchodilator therapy
Pneumonia
- Bronchial breath sounds over affected area (consolidation)
- Fine crackles that do not clear with coughing
- Increased vocal resonance (whispered pectoriloquy, bronchophony)
- Possible pleural rub if pleural inflammation present
COPD
- Generally diminished breath sounds
- Prolonged expiratory phase
- Wheezes and rhonchi, especially during exacerbations
- Barrel chest and hyperresonance to percussion
Pleural Effusion
- Diminished or absent breath sounds over fluid
- Dull percussion note
- Compressed lung above effusion may have bronchial breathing
- Egophony ("E" to "A" change) at upper fluid level
Integration with Other Clinical Data
Auscultation findings should always be interpreted in the context of:
- Patient history (smoking, occupational exposures, recent illness)
- Symptoms (cough, sputum production, dyspnea, fever)
- Other physical exam findings (respiratory rate, work of breathing)
- Vital signs (oxygen saturation, temperature)
- Laboratory and imaging results when available
Clinical Applications
Diagnosis
Breath sounds help differentiate between conditions such as pneumonia, bronchitis, asthma, and COPD.
Monitoring
Serial auscultation can track improvement or deterioration of respiratory conditions.
Response to Treatment
Changes in breath sounds may reflect effectiveness of interventions like bronchodilators, steroids, or diuretics.
Patient Education
Explaining auscultation findings helps patients understand their condition and adhere to treatment plans.
Case Examples
Case 1: Asthma Exacerbation
A 25-year-old female presents with acute shortness of breath and wheezing. Auscultation reveals diffuse expiratory wheezes throughout all lung fields with a prolonged expiratory phase. After bronchodilator therapy, breath sounds improve with minimal wheezing.
Clinical correlation: Reversible bronchospasm consistent with asthma exacerbation.
Case 2: Community-Acquired Pneumonia
A 60-year-old male presents with fever, productive cough, and right-sided chest pain. Auscultation reveals bronchial breath sounds and fine crackles in the right lower lobe with increased tactile fremitus.
Clinical correlation: Findings suggest consolidation consistent with pneumonia, later confirmed on chest X-ray.
Case 3: Pleural Effusion
A 70-year-old male with heart failure presents with increasing dyspnea. Auscultation reveals absent breath sounds at the right base with dullness to percussion. Above this area, there is egophony and bronchial breathing.
Clinical correlation: Findings suggest right-sided pleural effusion with compressed lung above it, confirmed by ultrasound.
Summary and Further Learning
Key Takeaways
- Lung auscultation is a fundamental clinical skill that provides valuable diagnostic information
- Normal breath sounds include vesicular, bronchial, and broncho-vesicular sounds, each with distinctive characteristics
- Abnormal breath sounds (wheezes, crackles, rhonchi, stridor, pleural rub) indicate specific pathological processes
- A systematic approach to auscultation ensures thorough examination
- Breath sounds should be interpreted in the context of the patient's clinical presentation
Further Learning Resources
Recommended Reading
- Bates' Guide to Physical Examination and History Taking
- Respiratory Physiology: The Essentials by John B. West
- Clinical Methods: The History, Physical, and Laboratory Examinations
- Auscultation Skills: Breath & Heart Sounds by Jessica Shank Coviello
- Sapira's Art and Science of Bedside Diagnosis
- The Principles and Practice of Medicine by William Osler
- Evidence-Based Physical Diagnosis by Steven McGee